02: Mother Nature is Not a Feminist
EP. 02
Studies looking at the natural history of aging in women show that once our estrogen levels start declining and we are no longer able to reproduce to support the species consistently, the conditions that can take us out of the gene pool start to rise. In short, Mother Nature is not a feminist. But with educating and advocating for ourselves, we can still thrive.
This episode gives an overview of what changes are starting and what you should look for in terms of symptoms once you hit the perimenopause transition, which can start as early as ages 35-40.
Listen to the full episode:
Are you feeling left in the dark about your body's natural aging process?
Many women feel lost when it comes to understanding the changes their bodies undergo as they age. When symptoms are brushed off by healthcare professionals, it can leave you feeling powerless.
But now is the time to reclaim the power and autonomy over our bodies! In this blog, I’m exploring the natural history of aging in women. Although we’ll see that Mother Nature isn’t exactly a feminist, we can still arm ourselves with the right knowledge to help us confidently advocate for ourselves when we meet with our healthcare providers.
Understanding Reproductive Health
One of the most important things for women to know is that we are born with a set number of eggs.
When we're tiny fetuses in the uterus (or in utero, as doctors say), our reproductive organs haven't fully formed yet. This is when the ovaries start developing follicles, tiny structures that contain immature eggs. By week 20 in utero, our reproductive systems are fully formed, and at that point, we have about six to seven million eggs in our ovaries. Yes, you read that right – millions!
But by the time we're born, that number has already dropped to one to three million. And before we have even taken our first breath, our egg count has significantly decreased. As we go through life, our egg count continues to drop. By the time we hit our menstrual periods, we're down to around 400,000 eggs on average and when we reach our thirties, it's gone down to the 100,000 range.
From this, you can see that fertility declines over a period of time and menopause happens when we run out of eggs - that's traditionally how it's been defined (although it is a bit more complicated and nuanced than that).
The Role of Hormones
Our ovaries are like puppets controlled by a gland in our brain: the pituitary gland. And this gland acts as the remote control for most of our endocrine organs, sending signals to various parts of our body, including our ovaries.
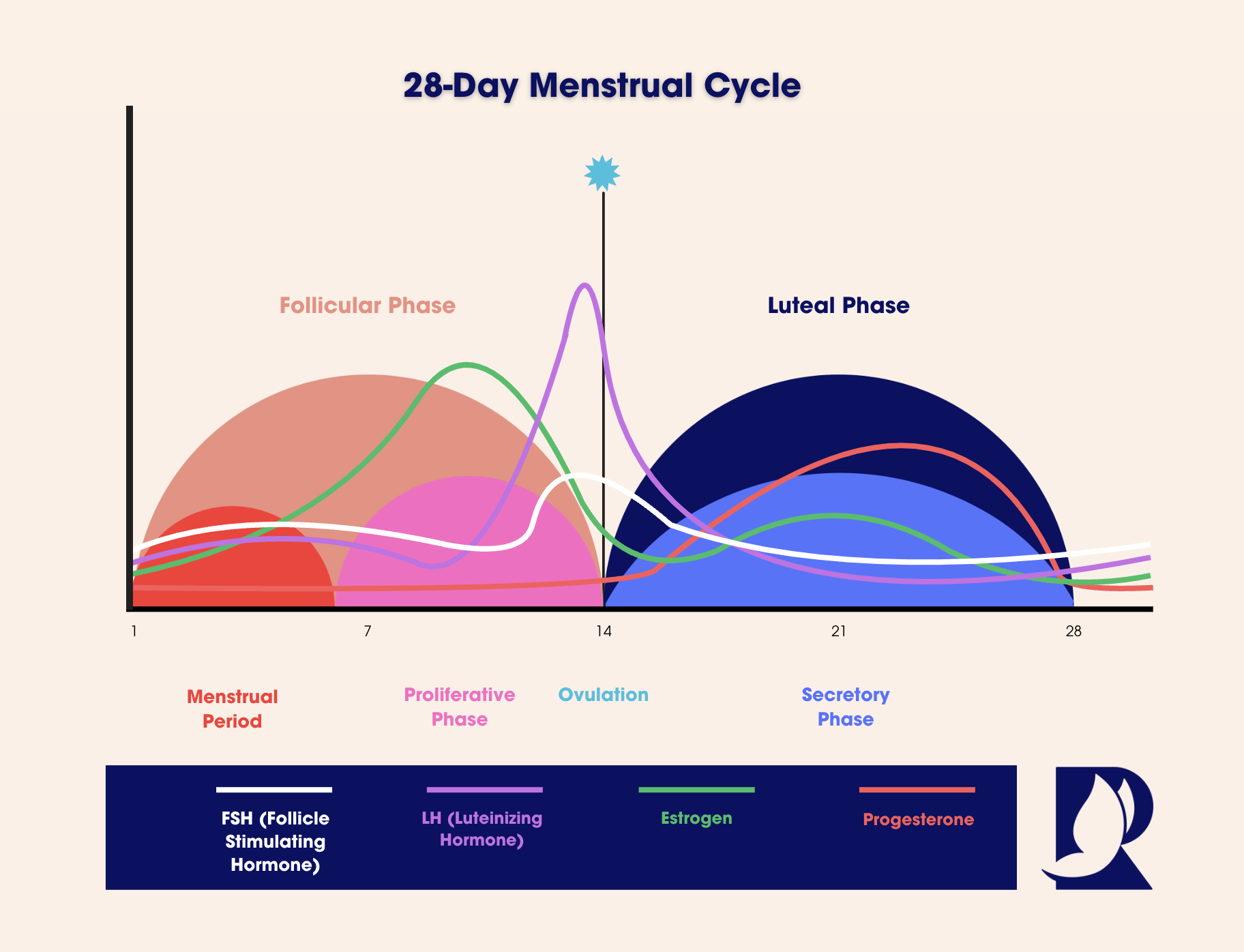
In a regular menstrual cycle, these signals, known as FSH and LH, cause changes in the lining of our uterus and the release of eggs from our ovaries. If an egg is fertilized, it implants in the uterus and develops into a pregnancy. If not, we have another menstrual period, and the cycle starts again.
The Menstrual Cycle
The menstrual cycle is divided into phases, with the follicular phase being the first. This is when we have our period, and estrogen levels start to rise. Around day 14, we ovulate – the ovaries release an egg – thanks to a spike in LH and FSH.
In the second half of the menstrual cycle (the luteal phase), progesterone levels start to rise to prepare that lining for the potential of a fertilized egg. If the egg is fertilized and implants, then the progesterone continues to rise and you will theoretically go into a pregnancy. If it doesn't, progesterone levels drop, and the uterine lining sheds, marking the start of a new cycle.
(It's important for women to understand that in science, we look at cycles based on 28 days, even though there is a lot of variation in the length of people’s cycles.)
Phases of Menstrual Cycle
Navigating Midlife Hormonal Changes
As our egg count declines over our lifetime, we eventually reach a point where it bottoms out. This marks the onset of what's known as midlife or perimenopause transition. It's a period characterized by significant shifts in our bodies and one of the most noticeable changes is the cessation of periods, known as menopause. But this phase isn't just about the end of menstruation – it's a time of profound hormonal fluctuations that can impact our health and well-being.
Estrogen and Progesterone
During midlife, estrogen and progesterone levels start to decline alongside egg count. These hormones play crucial roles in regulating menstrual cycles and maintaining the health of reproductive organs. Menstrual cycles become more irregular as their levels decrease, leading to unpredictable periods. Eventually, estrogen and progesterone levels bottom out, and menstruation ceases altogether.
Defining Midlife
Midlife isn't just a specific age—it's a stage of life characterized by hormonal changes and transitions. Many women experience symptoms like hot flashes, night sweats, mood swings, and changes in libido during this time. Understanding these hormonal shifts can help us navigate this phase more easily and empower us to advocate for our health.
Hormonal Shifts through Perimenopause to Postmenopause
Metabolic Changes During Midlife
If you look at this purely from a biological perspective, when we are not reproducing consistently, we're not contributing to the gene pool. So Mother Nature thinks we’re not really helping her out. And when our estrogen and progesterone levels are declining, she's ready to exit us out from the system (not such a happy thought!).
When you look at all of the metabolic changes that start happening in this time period, it’s fairly clear that Mother Nature is *not* a feminist! These are some of the key metabolic changes women can experience:
Muscle Mass Decline: As our estrogen, progesterone, and possibly testosterone levels decline, our bodies start losing muscle mass. This loss of muscle mass affects our metabolism, making it harder to maintain a healthy weight.
Increase in Fat Mass: We start gaining fat, especially around our middle. This visceral fat not only affects our appearance but also increases our risk of heart disease, stroke, and diabetes.
Elevated Blood Pressure and Cholesterol: With weight gain and changes in hormone levels, our blood pressure and cholesterol levels tend to rise, further increasing our risk of heart disease and other cardiovascular issues.
Rise in Blood Sugar: Excess fat around our abdomen leads to insulin resistance, causing blood sugar levels to increase. This puts us at higher risk of developing diabetes.
Bone Density Decline: Muscle loss also affects our bones, leading to a decrease in bone density. This makes our bones more prone to fractures, with hip fractures being particularly concerning due to their high mortality rate in older adults.
Sleep Disturbances: Many women experience difficulty sleeping during midlife, either due to hormonal changes or other factors like hot flashes. These disturbances can impact our overall well-being and quality of life.
Pelvic Floor Weakness: Muscle mass loss affects the pelvic floor muscles, leading to issues like urinary incontinence, urinary tract infections, vaginal dryness, and pain during intercourse. These issues can have a significant impact on our quality of life and overall health.
As these changes accumulate, we may notice a decline in our quality of life and overall longevity. Just a few generations ago, our ancestors didn't have the benefit of the scientific and medical advancements that we enjoy today. Back then, life expectancy was shorter, and people typically didn't live as long as we do now. Previously, if someone lived to around 65 years old, they might only have had to contend with these symptoms for a decade or so after menopause. However, with modern advancements, we're now looking at another several decades of life after menopause. This longer life span highlights just how vital it is to take an active role in maintaining our health.
It's also crucial to be aware of your family history and genetics, as these factors can influence your experience of menopause. We're all unique in terms of our genetic makeup, and what one person experiences during menopause may differ from another. Pay attention to any symptoms you may be developing, as early detection and intervention can make a significant difference in managing menopausal symptoms and maintaining your health.
When visiting healthcare providers, don't hesitate to speak up and ask questions. Advocate for yourself and ensure that your concerns are addressed. It's essential to have open and honest conversations with your healthcare team to receive the support and care you need during this transition. By taking proactive steps and staying informed, we can navigate menopause with confidence and embrace this new chapter of life with vitality and well-being.